Safe Feeding Advice
Please note: this advice is for care home staff
A person is much more likely to develop aspiration pneumonia if they need someone to feed them. The following advice is for residents who need support with feeding.
| Level of alertness | No-one should be given food or drink if they are not fully alert. |
| Distractions |
Reduce distractions when eating and drinking. If your resident is easily distracted, consider moving them to a quiet place during mealtimes, with less background noise and chat. Help them to focus on eating and drinking if they become distracted. |
| Time |
Do not rush mealtimes. Make sure there is enough time to support the person to eat and drink. If they take a long time to eat, keep their food and drink warm (or cold) in insulated containers. |
| Positioning |
Sit people fully upright (90o, with head in neutral position) for all snacks, meals and drinks. If they are in bed, raise the bed head and use pillows to keep them upright. They need to stay upright for at least half an hour after a meal to avoid reflux. If it’s difficult to keep them in the right position, consider a referral to physiotherapy to help with this. |
| Oral Hygiene and pneumonia |
Dental plaque contains many different kinds of bacteria and some of them can cause pneumonia. People with eating and drinking difficulties may aspirate (breathe in) their oral and throat secretions. Excellent oral hygiene will help reduce the risk of chest infections and pneumonia. Make sure the mouth is clean and free from residue at the end of the meal. Mouth care should be given at least twice per day. Dentures should be removed and cleaned daily. Download our 'Mouthcare for People with Swallowing Difficulties' leaflet by clicking here. |
| Position yourself |
Sit at eye level and facing the person you are assisting. |
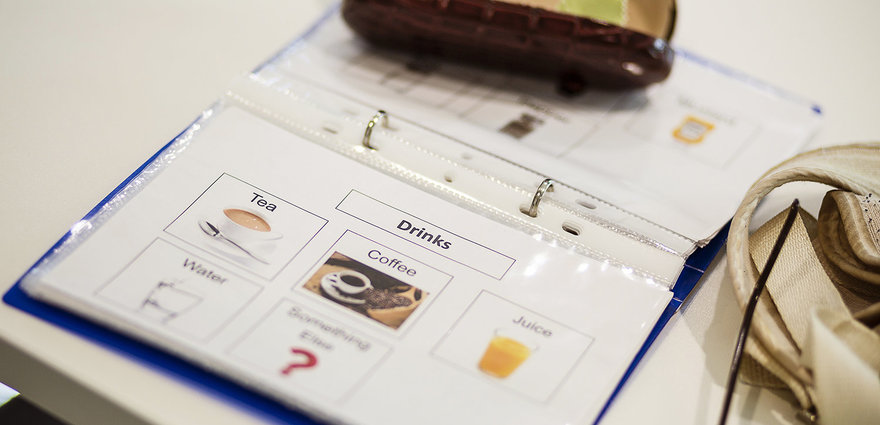
| Utensils |
Are you using the right utensils? Try different sized and adapted cutlery to see if the person can manage these more easily. Try normal cups and glasses first. Don’t automatically use spouted beakers or straws. These should only be used if recommended or there is evidence of a real need as they may cause more problems with swallowing. |
| Teeth |
If the person wears dentures they should fit well. Please ensure they are seen by a dentist if any concerns over their teeth. If they have problems chewing due to lack of teeth, they may be better with softer foods. Unless they have swallowing problems, they won’t need a referral to our service. |
| Glasses and hearing aids |
Should be worn when eating and drinking. Talk to the person and let them know what the meal is and when you are offering the next spoonful. |
| Modifying Diet |
Make sure you are giving the most appropriate diet for their needs. If they are having problems swallowing or spitting out lumps, they may need softer or smoother textures. Refer to Speech and Language Therapy if unsure what to provide. Follow any modified diets recommended by a Speech and Language Therapist. Food should look appetising and smell appealing to stimulate the appetite. |
| Independence |
People should be encouraged to feed themselves. Don’t assume they need full assistance. If they are having problems holding a cup, they may need a handled beaker or hand over hand assistance. If they are having problems with a knife or fork, they may manage better with a spoon or be able to self feed if you load the spoon for them. |
| Size of mouthful |
Try different sized mouthfuls. The mouthful should be enough to stimulate chewing and swallowing; avoid very big mouthfuls. People feeding themselves may need reminding not to put too much in their mouths and to finish each mouthful before taking the next. |